Virtual Health Replaced Some In-Person Visits, But Can It Transform Health Care?
While virtual health has the potential to transform the way care is delivered, it’s too soon to know if that potential will be realized. The shift from paper medical records to electronic medical records (EMR) promised a similar transformation, yet has not fully captured the benefits of a digital platform.
Nevertheless, since the pandemic emerged, virtual health has reached a point where it could become more than a substitute for in-person visits. If done well, virtual health could help transform care delivery. This transformation is necessary and can meet the needs of patients more effectively, keep them healthier, and respond to different drivers of health to ensure equitable care.
Four dimensions of virtual health transformation
We identified four dimensions health care organizations can use to evaluate the types of care offered virtually, conditions treated virtually, and considerations to be given to the drivers of health when integrating virtual health into new care pathways.
1. Type of care: Primary care and some specialty care (e.g., behavioral health and dermatology) are well suited for virtual health. These types of care tend to revolve around clinician-patient interactions, which can typically be replicated virtually. A clinician, for example, might be able to assess a skin condition by reviewing an online image that the patient took with a smartphone. However, some specialties, such as oncology or orthopedics, have clinical intricacies limiting virtual health to areas such as post-operation assessments. In-person care is sometimes unavoidable when diagnoses need to be explained (e.g., oncology) or when examinations cannot be replicated virtually (e.g., gait analysis). However, while virtual health still might supplement in-person interactions (e.g., routine labs follow-ups during chronic oncology care), organizations will need to be deliberate when determining how to most effectively combine in-person and virtual care.
2. Complexity of care: Complexity is the level of clinician involvement required to effectively serve the patient and is closely linked to the type of care and the setting. Lower-touch care does not typically require a live interaction, can be delivered anywhere, and is usually associated with stable patients. Higher-touch care is required for more complex cases and usually requires the clinician to meet with the patient in-person. Given the greater complexity, the limitations of virtual health may make it difficult for a clinician to properly evaluate the patient. Medium-touch care sits in between low- and high-touch care and usually requires some form of synchronous or asynchronous provider-patient interaction.
3. Purpose of care: Virtual health can be used to prevent, manage, and treat illnesses as well as monitor patients in recovery. Effective prevention and management require empowering the patient while enabling greater convenience. Digital-engagement applications and self-service tools can help patients track their diet, post patient-reported outcomes, or quickly check-in with a health coach. Integrating these tools can help patients achieve various care goals. However, treatment can be complex and sometimes requires specialist oversight. In these cases, virtual health can extend access to specialists at the point of care.
4. Drivers of health: Health care organizations need to understand the patient’s drivers-of-health profile (i.e., social, economic, and environmental conditions) and determine whether it enables or inhibits the application of virtual health. For instance, virtual health has little value for a patient who doesn’t have access to a stable internet connection, but may have immense value for a patient looking to reduce the burden of traveling to in-person visits. Properly understanding the risk profile of patients is critical to determining whether newly designed virtual care pathways are appropriate at the patient level.
A decision set for virtual health transformation
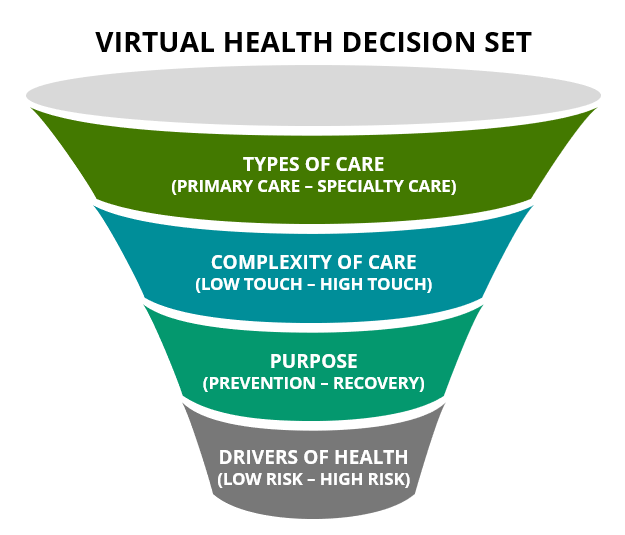
We recommend that health care organizations assess each dimension from the top down. The dimensions at the top will help determine the types of specialties and services best suited for virtual health, often based on their volume and frequency. The dimensions at the bottom account for more patient-specific considerations and are equally critical to enabling care model transformation.
Early in the pandemic, virtual visits were treated as a substitute for in-person visits. The urgent need to adjust to the situation and the unique regulatory pressures lifted allowed organizations to see firsthand how virtual care could be used. We now have a great opportunity to leverage those learning and take them a step further.
Blog Authors:
Urvi Shah, senior manager, Deloitte Consulting LLP
Elizabeth Baca, M.D., M.P.A., specialist leader, Deloitte Consulting LLP
Acknowledgments: Zach Miller, Sonal Purohit

